Being diagnosed with herpes simplex virus (HSV), particularly HSV-2, can have a significant emotional impact.
The diagnosis often triggers feelings of distress, anxiety, and lowered self-esteem, as many people struggle to come to terms with the chronic nature of the infection and concerns about transmission and relationships.
HSV-2, which primarily causes genital herpes, tends to carry a heavier emotional burden compared to HSV-1 due to its association with sexual transmission and social stigma.
This can lead to increased feelings of shame and isolation, especially soon after diagnosis.
Stigma around Herpes in the US and Worldwide
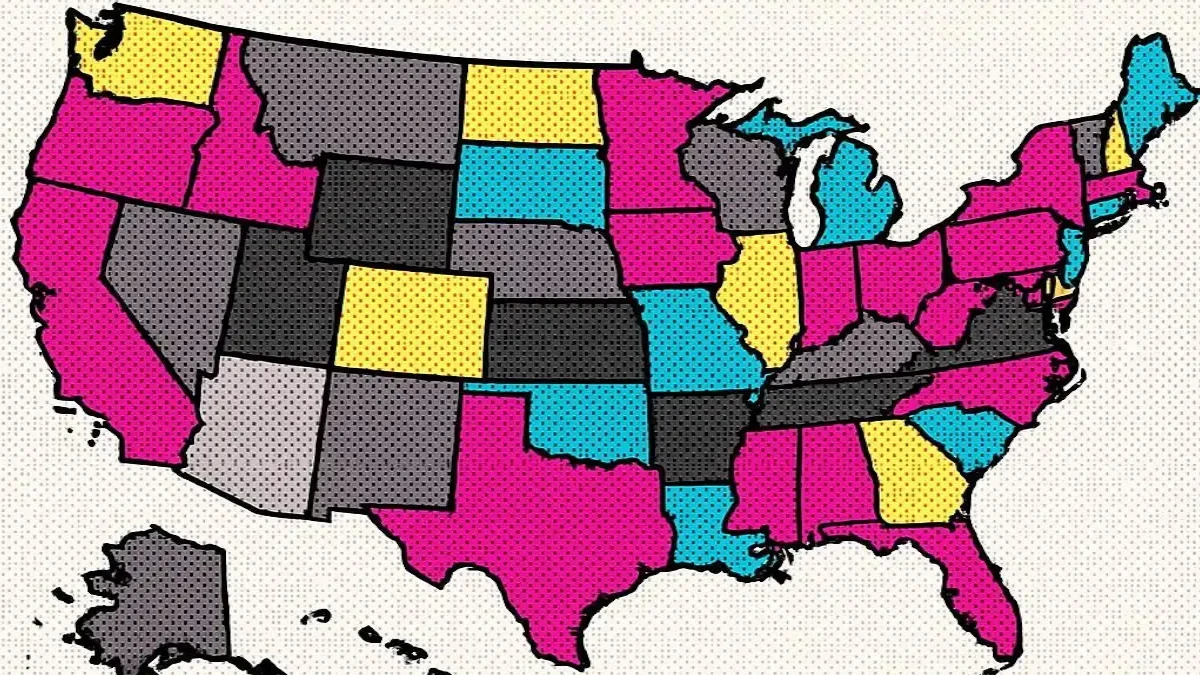
The stigma surrounding herpes is particularly widespread and intense in the United States, where misconceptions and negative attitudes often exacerbate emotional distress for those living with HSV.
In contrast, many countries in Europe and other parts of the world tend to have a more casual or accepting view of herpes, especially HSV-1, which causes oral cold sores and is extremely common.
HSV is actually one of the most widespread viruses globally, with the majority of people carrying either HSV-1 or HSV-2, often unknowingly.
This high prevalence means that herpes is a normal part of human viral ecology, yet stigma persists largely due to misinformation and cultural attitudes.
Common Emotional Responses to an HSV Diagnosis
Following an HSV diagnosis, it is common to experience a range of intense emotions including shock, embarrassment, anxiety, and fear.
Many individuals worry about how the diagnosis will affect their social life, intimate relationships, and self-image.
These feelings can sometimes lead to depression, social withdrawal, and difficulties with disclosure to partners or friends.
Women often report higher levels of psychological distress related to herpes, which may be influenced by societal expectations and gender norms.
Understanding that these emotional responses are normal and shared by many can help reduce feelings of isolation and encourage seeking support and education to better manage both the physical and emotional aspects of herpes.

Stress has long been considered a trigger for herpes outbreaks, but recent research reveals a more nuanced relationship.
While stress can contribute to the frequency and severity of outbreaks, the presence of herpes symptoms themselves often leads to increased stress and emotional distress, creating a vicious cycle.
Managing stress through techniques such as mindfulness, exercise, adequate sleep, and counseling can be crucial not only for emotional well-being but also for potentially reducing the occurrence of outbreaks.
Neurological and Psychiatric Associations with Herpes Viruses
Emerging studies suggest that certain herpes viruses, including HSV-1 and human herpesvirus 6 (HHV-6), may have effects beyond the skin, potentially impacting the nervous system and mental health.
Research has linked HSV-1 infection with an increased risk of psychiatric disorders such as depression and bipolar disorder, as well as suicidal behavior in some populations.
HHV-6 has also been implicated in neurological conditions and mood disorders.
While these associations do not imply causation for everyone, they highlight the importance of considering herpes infections within a broader mental health context and the need for integrated care approaches.
Effective Coping Strategies and Support for Mental Health
Addressing the mental health challenges related to herpes requires a holistic approach.
Antiviral treatments can reduce outbreaks and physical symptoms, which often helps alleviate associated emotional distress.
Psychological support such as cognitive-behavioral therapy (CBT), stress management techniques, and participation in support groups can provide valuable tools for coping with anxiety, depression, and stigma.
Open communication with partners and trusted individuals fosters understanding and reduces feelings of isolation.
Education about the widespread nature of HSV also helps normalize the condition and diminish shame.
Building Healthy Relationships with Herpes
Maintaining healthy intimate relationships after an HSV diagnosis can be challenging but is entirely possible with honest communication and mutual understanding.
Disclosing your herpes status to partners can feel daunting, but it fosters trust and helps manage expectations.
Using protection methods such as condoms and antiviral therapy can significantly reduce transmission risk, allowing for fulfilling and safe relationships.
Support from partners and open dialogue play a crucial role in reducing anxiety and strengthening emotional bonds.
Reducing the stigma associated with herpes is essential for improving mental health outcomes for those affected.
Public education campaigns and open conversations can dispel myths and normalize HSV as a common viral infection.
Encouraging empathy and understanding within communities helps create supportive environments where individuals feel comfortable seeking help and discussing their experiences without fear of judgment.
If feelings of anxiety, depression, or social isolation related to herpes become overwhelming or interfere with daily life, it is important to seek professional support.
Mental health professionals can provide counseling, therapy, and coping strategies tailored to your needs.
Additionally, if herpes outbreaks are frequent, severe, or complicated by other health issues, consulting a healthcare provider for medical management is crucial.
Combining medical and psychological care offers the best approach to overall well-being.
Mental Health and Herpes FAQs
How does an HSV-2 diagnosis affect emotional well-being?
An HSV-2 diagnosis can cause significant emotional distress, including feelings of shame, anxiety, and lowered self-esteem, due to its association with genital herpes and social stigma.
Why is herpes stigma more intense in the United States compared to other countries?
In the United States, herpes stigma is particularly widespread because of cultural attitudes and misinformation. In contrast, many European countries have a more casual acceptance of HSV, especially HSV-1, which is very common globally.
Can stress trigger herpes outbreaks?
Stress can contribute to outbreaks, but herpes flare-ups themselves often increase stress, creating a complex cycle. Managing stress is important for both mental health and outbreak control.
Are herpes viruses linked to mental health disorders?
Some studies suggest that HSV-1 and other herpes viruses may be associated with an increased risk of psychiatric disorders such as depression and bipolar disorder, highlighting the need for integrated care.
What strategies can help cope with the emotional impact of herpes?
Effective coping includes antiviral treatment, psychological therapies like cognitive-behavioral therapy (CBT), stress management, support groups, and open communication with partners and loved ones.
When should I seek professional mental health support?
If feelings of anxiety, depression, or isolation become overwhelming or interfere with daily life, professional counseling or therapy can provide essential support and coping tools.
Bravado Labs Advanced Lysine Immune Boost
Why we love it:
- Verified Customer Favorite
- High Quality Ingredients
As an affiliate, we earn from qualifying purchases.
Recommended Supplements for Herpes Management
Simplix Viral Defense
Cold Sore & HSV Support
Simplix Viral Defense
Cold Sore & HSV Support
Synergistic formula combining L-Lysine, shiitake mushroom, and marine bioactives for comprehensive immune support.
SHOP NOW & SAVE 15%